Folliculitis affects people of all ages, from babies to the elderly. It can be caused by different factors like bacteria and fungi. Knowing the difference between bacterial and fungal folliculitis is key. The treatments for each vary a lot. This skin issue can show up anywhere on the body. But knowing what causes it on the scalp is vital for good care and stopping worse problems.
A study looked at 100 people with folliculitis. The study found that getting the right diagnosis is crucial to start the correct folliculitis treatment. Out of them, 20 had Malassezia folliculitis, and 80 had other forms. Later, 16 cases thought to be non-Malassezia were found to be Malassezia after all. This shows the challenges doctors face. Not telling bacterial from fungal types apart can lead to wrong treatments. This could make the patient’s condition worse, highlighting the need for right diagnosis.
By reading about this topic, the reader will learn about how common both conditions are. They will understand the symptoms of each type and how to diagnose them properly. This knowledge is the first step towards better treatment and prevention as they deal with folliculitis.
Key Takeaways
- Folliculitis is a common condition affecting all age groups.
- Accurate diagnosis is essential for effective treatment.
- Notably, scalp folliculitis may be influenced by several factors, including shaving and skin hygiene.
- Appropriate treatment varies significantly between bacterial and fungal causes.
- Monitoring and preventive measures can help reduce recurrence.
Understanding Folliculitis
Folliculitis is when hair follicles get inflamed, causing red, itchy bumps. These can look a lot like acne. It’s caused by things like infections, shaving irritation, or tight clothes. Knowing what causes folliculitis helps recognize its symptoms and find good treatments.
Some common symptoms are pustules on hair follicles, pain, and itching. It makes daily activities tough. Lesions often pop up after shaving or using a contaminated hot tub. Spotting these folliculitis symptoms is key to getting the right diagnosis. Often, a bacterium called Staphylococcus aureus is the culprit. But, yeast like Malassezia can cause it too.
Risk factors include shaving, tight clothes, curly hair, or using dirty hot tubs. People with acne or those on long-term antibiotics might get it more often. Taking care of your skin can really help manage it.
If you want to learn more about dealing with folliculitis, check out this helpful guide.
Common Causes of Folliculitis
Folliculitis is a skin condition often caused by infections. It’s common and involves the Staphylococcus aureus bacteria. This bacteria infects hair follicles. This type is seen a lot, especially in people who’ve had it before.
Fungal folliculitis is linked to yeast, mainly the Malassezia species. Hot, wet weather, oily skin, and some skincare products can increase its growth. These elements make a perfect spot for fungi to live.
Many things can raise your chances of getting folliculitis. These include:
- Being overweight makes you more likely to get it.
- Shaving or waxing can harm the skin and follicles.
- Tight clothes create a warm, moist place for germs to grow.
- Poorly cleaned hot tubs can cause hot tub folliculitis from Pseudomonas aeruginosa.
- Using antibiotics for a long time can harm your skin’s natural defenses.
Here’s a table showing the main types of folliculitis:
| Type of Folliculitis | Cause | Common Symptoms |
|---|---|---|
| Bacterial Folliculitis | Staphylococcus aureus | Red bumps, pus-filled blisters, itching |
| Fungal Folliculitis | Yeast (Malassezia) | Itchy, red bumps, flakiness |
| Hot Tub Folliculitis | Pseudomonas aeruginosa | Sooty red bumps in covered areas |
| Pityrosporum Folliculitis | Yeast overgrowth | Itchy, inflamed hair follicles |
If you’ve had folliculitis, you might get it again. But you can prevent it. Keep clean, wear loose clothes, and shave carefully. Doing these can help stop bacterial and fungal folliculitis.
Folliculitis Symptoms and Initial Diagnosis
Folliculitis symptoms often include red bumps or pustules on the scalp. People might feel itching or pain where it shows up. These folliculitis symptoms usually point to inflamed hair follicles, caused by bacterial or fungal infections.
The first step in diagnosis is usually checking the patient and their medical history. Doctors look for how the lesions group together. Recognizing these symptoms helps figure out if the infection is bacterial or fungal. It’s important to get this right because different types look similar.
Sometimes, more tests are needed. This could mean skin scrapings, cultures, or biopsies if things don’t improve. Knowing all about folliculitis symptoms is key to the right treatment. This helps avoid worse problems like spreading infection, scars, or losing hair.
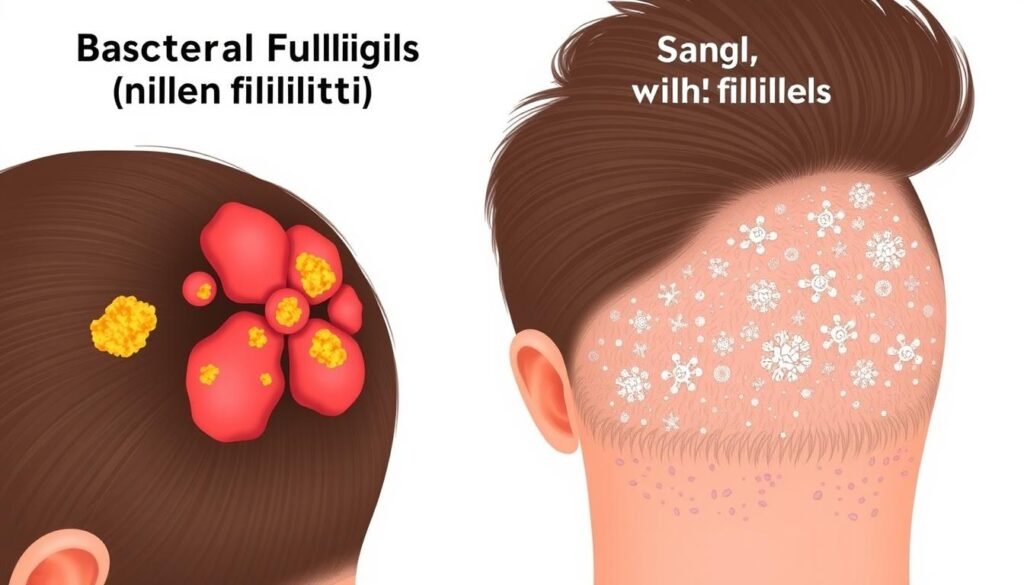
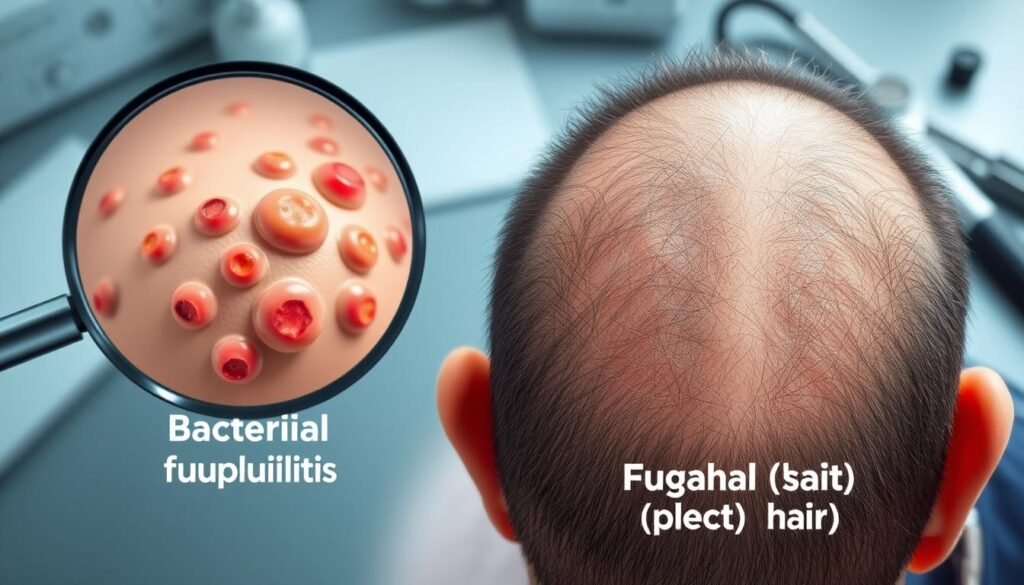
Differentiating Between Bacterial and Fungal Folliculitis
To tell bacterial and fungal folliculitis apart, it’s crucial to look at their signs. Bacterial folliculitis usually shows up as red, painful bumps that can really bother you. This kind tends to happen when staphylococcus bacteria infect the skin. Thankfully, antibiotics often work well to treat this infection.
Fungal folliculitis, on the other hand, is caused by too much Malassezia yeast. This leads to small, itchy bumps that you might see on your arms, chest, and back. One key to spotting fungal folliculitis is by its intense itch, something not common in bacterial cases.
| Characteristic | Bacterial Folliculitis | Fungal Folliculitis |
|---|---|---|
| Cause | Staphylococcus bacteria | Malassezia yeast |
| Symptoms | Red, painful pustules | Small, itchy, dome-shaped papules |
| Treatment | Antibiotics | Antifungal medications |
| Location | Commonly on the scalp and face | Typically on arms, chest, and back |
| Itching | Rare | Common |
Knowing the difference between the two is key for doctors. It helps them pick the right treatment for each condition. Making the right diagnosis is super important in treating bacterial and fungal folliculitis right.
How Can You Tell If Folliculitis Is Bacterial or Fungal?
It’s important to know if folliculitis is caused by bacteria or fungus. Each has different folliculitis symptoms. These signs help tell them apart.
Recognizing the Signs of Bacterial Folliculitis
Bacterial folliculitis shows up as:
- Pronounced inflammation and redness
- Pus-filled white bumps on the skin
- Occasional pain or tenderness in the affected area
- Fast onset, especially after skin injuries or shaving
- Potential for scarring if untreated
These signs help diagnose bacterial folliculitis. Then, antibiotics can be used to treat it.
Identifying Symptoms of Fungal Folliculitis
On the other hand, fungal folliculitis shows:
- Less pronounced inflammation
- Widespread itchiness across the affected area
- Clusters of small red or skin-colored bumps
- Symptoms that may appear after hot tub use or in humid conditions
- Recurring episodes, suggesting a persistent fungal infection
Different signs help spot folliculitis symptoms caused by fungi. Treating it often requires antifungal medicines. Knowing these symptoms leads to better management of the condition.
Diagnostic Methods for Folliculitis
A healthcare professional usually starts diagnosing folliculitis with a detailed check-up. They will ask about your medical history and look closely at the affected area. Spotting signs of infection early helps make a clear folliculitis diagnosis.
To tell bacterial from fungal folliculitis, certain tests are key. Doctors often scrape the skin to look for yeast. This step is crucial for spotting fungal infections tied to Malassezia fungi.
Sometimes, they’ll swab the area to see if bacteria are to blame. For tricky cases, a skin biopsy can make things clearer. Though not common for folliculitis, a biopsy helps when the usual tests don’t give answers.
If you have a mild case, taking care of it at home might work. Try a warm washcloth and over-the-counter antibiotics if needed. Knowing when to see a doctor about folliculitis is important.
Choosing the right treatment depends on the folliculitis type. Antifungal medicines are used for fungal issues. But for bacteria or mites, treatments differ.
Being part of your care is crucial. Ask questions and share your symptoms openly. This way, you get the best folliculitis diagnosis and treatment.
Effective Treatments for Bacterial Folliculitis
Bacterial folliculitis needs specific folliculitis treatment to ease symptoms and stop worse problems. It’s often caused by Staphylococcus aureus, a common germ. Doctors usually treat it with antibiotics first.
For fast relief, lotions like clindamycin help calm the redness. If it’s really bad, drugs like cephalexin might be used all over the body. This is especially true if lotions aren’t doing the trick.
There are different kinds of bacterial folliculitis. Each one comes from different things and needs its own treatment strategy:
| Type of Folliculitis | Common Causes | Treatment Options |
|---|---|---|
| Staphylococcal Folliculitis | Staphylococcus aureus infection | Topical clindamycin, systemic antibiotics |
| Hot Tub Folliculitis | Pseudomonas aeruginosa in poorly sanitized hot tubs | Antibiotics, maintain proper hygiene |
| Pseudofolliculitis Barbae | Shaving against hair growth | Avoiding shaving techniques, topical treatments |
| Irritant Folliculitis | Shaving, waxing, or tight clothing | Gentle skin care, topical treatments |
| Drug-Induced Folliculitis | Certain medications (e.g., corticosteroids) | Stop medication under medical guidance |
Getting the right diagnosis is key to treating folliculitis treatment well. If you’re having ongoing issues, see a doctor. They’ll make a treatment plan to reduce swelling and keep more outbreaks at bay. The aim is to keep your skin healthy.
Effective Treatments for Fungal Folliculitis
Treating fungal folliculitis means finding the right therapies. These treatments aim to kill the fungus and ease symptoms. Many suffer from Pityrosporum folliculitis, leading to itchy spots. It’s crucial to know which kind you have to avoid treatments that don’t work.
Use of Antifungal Medications
Oral antifungals are top picks for beating Pityrosporum folliculitis. Doctors often suggest Sporanox (itraconazole) or Nizoral (ketoconazole). These are used for one to three weeks.
For not-so-severe cases, Nizoral shampoo or Selsun might help. These have selenium sulfide. If there’s little change, stronger options like oral isotretinoin could be needed. Regular treatment may go on twice or thrice a week for one to two months after starting. This helps keep the condition from coming back.
Importance of Proper Diagnosis for Treatment
Getting the diagnosis right is key for treating folliculitis well. Wrong diagnoses often lead to using antibiotics that don’t work for fungal issues. This can make things worse. Knowing the risks like antibiotic use, diabetes, and stress is important. These factors can raise the chances of getting Pityrosporum folliculitis. Without pinpointing the correct cause, treatments might not work, letting the condition linger or get worse.

Preventive Measures Against Folliculitis
Effective management of folliculitis starts by keeping clean. Wash your scalp often with a gentle cleanser. This helps take away dirt, oil, and things that might irritate the skin. Stay away from products that may block hair follicles and cause irritation. Keeping clean doesn’t just lower the chance of infections. It also helps your scalp stay healthy.
What you wear matters too. Choose clothes that are not tight. This can reduce rubbing against your skin and lessen irritation. Try not to touch or scratch areas that are already bothered. Doing so can make things worse and might lead to more infections.
To sum up preventive steps, check these out:
- Maintain clean, moisturized skin to avoid folliculitis outbreaks.
- Use proper shaving techniques to prevent irritation, important for those who get pseudofolliculitis barbae.
- Avoid skin irritants, like heavy creams and oils that can trigger folliculitis.
- Keep personal items, like razors and washcloths, clean to avoid germs.
- Stay away from hot tubs with dirty water, as they can have bacteria causing hot tub folliculitis.
By following these tips, you can take charge of your scalp’s health. This cuts down the risk of getting folliculitis again. Knowing how to manage folliculitis helps you keep a healthy scalp. It’s all about taking the right steps before problems start.
Conclusion
Knowing how to tell bacterial from fungal folliculitis is key to treating scalp infections right. Bacterial infections have different symptoms than fungal ones. For example, Staphylococcus aureus causes different problems than Tinea Capitis, which can make your skin scaly and make you lose hair. Spotting these signs early helps people get the right help and keeps bad things, like losing hair for good, from happening.
To properly diagnose this, doctors do a full check and might run extra tests. This helps them figure out the best way to fix the problem. If you’re not getting better or if things seem off, see a doctor right away. They’ll give advice that fits just you, making it easier to handle folliculitis.
Learning about folliculitis and how to deal with it makes for healthier skin and lowers infection chances. Being proactive, cleaning your hair well, and knowing how to care for your scalp are big steps towards prevention. For tips on keeping your scalp healthy, visit this page on folliculitis management.
