Buttock folliculitis makes up 25-35% of all folliculitis cases. Many think it’s just butt acne, but it’s more than that. It’s an inflammation of hair follicles, causing discomfort and self-awareness. Knowing what causes and signals butt folliculitis is key for those with red, sore bumps.
Many things can cause it, like bacterial infections and too much friction from clothes. There are also other health issues involved. This piece aims to enlighten readers about butt folliculitis. It talks about the best treatments and simple ways to take care of your skin. For more info on folliculitis, check out this page.
Key Takeaways
- Butt folliculitis, frequently confused with butt acne, primarily affects hair follicles.
- Friction, sweat, and certain clothing choices contribute significantly to the condition’s development.
- Symptoms include red and inflamed bumps, itching, and possible pus-filled lesions.
- Effective treatments range from at-home remedies to medical options like antibiotics or antifungal medications.
- Preventative measures include maintaining proper hygiene, choosing breathable fabrics, and following a consistent skincare routine.
Understanding Butt Folliculitis
Butt folliculitis is a skin issue that happens when hair follicles get inflamed or infected. It can cause discomfort and visible lesions. Defining folliculitis helps us see it mainly involves hair follicles, not skin pores. This makes it different from other conditions it’s often confused with.
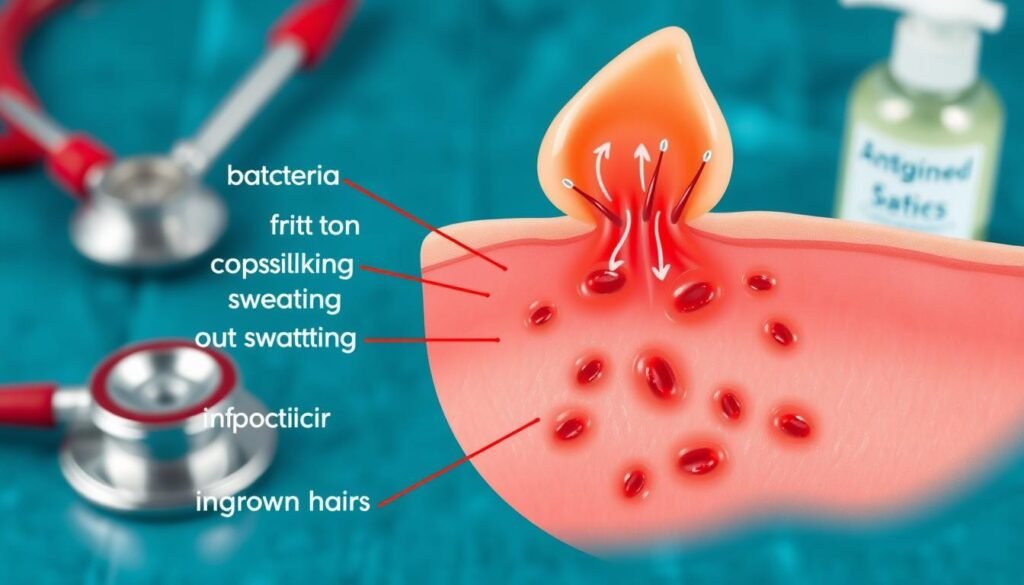
Definition of Folliculitis
Folliculitis is common, especially on the buttocks because of many hair follicles there. It appears as red bumps or pus spots. The main causes include friction, too much sweat, and bacteria, especially Staphylococcus aureus. These factors help explain the development of butt folliculitis.
How Butt Folliculitis Differs from Other Skin Conditions
In comparing skin conditions, butt folliculitis is often mixed up with butt acne. But, butt folliculitis starts in hair follicles. Conditions like keratosis pilaris and boils look similar but stem from other problems. Keratosis pilaris features painless bumps that can get better with time. Unlike folliculitis, which can be tender and flare up due to irritation or infection. Knowing these differences is key for the right treatment.
Causes of Butt Folliculitis
Knowing why butt folliculitis happens is key to stopping and treating it. Several things cause it, like bacterial infections, chaffing and sweating, the type of clothes you wear, and health issues.
Bacterial Infections
Bacterial infections, mainly by Staphylococcus aureus, are a big cause. This bacterium is found on up to 30% of people’s skin and can infect hair follicles. People with weak immune systems or diabetes have a 2 to 3 times greater risk of getting these infections, making folliculitis more likely.
Friction and Sweat
Friction and sweat heavily contribute to butt folliculitis. Sweat happens for 60-80% of adults during exercise or in warm weather. This moisture worsens the condition. Also, skin rubbing against clothes or itself, especially on the buttocks, invites infection. Prolonged sitting makes things worse for about 80% of office workers.
Impact of Clothing Choices
The wrong clothes increase the risk of butt folliculitis. Tight and synthetic clothes cause a lot of friction. About 40-50% of people wearing them experience more acne in the buttocks area. Looser clothes can help lower this friction, cutting down on outbreaks by around 30%.
Underlying Health Conditions
Health issues also play a role in butt folliculitis. Having recent skin injuries, like cuts, ups your risk by 1.5 times. Also, things like hormone shifts and what you eat can affect skin health. This leads to a higher chance of getting folliculitis.
| Contributing Factor | Impact on Folliculitis Risk |
|---|---|
| Bacterial Infections | Up to 30% of people carry Staphylococcus aureus; higher risk for those with weakened immune systems. |
| Friction and Sweat | 60-80% of adults sweat during activities, with prolonged sitting increasing susceptibility. |
| Clothing Choices | Tight and synthetic fabrics increase irritation, affecting up to 50% of individuals. |
| Underlying Health Conditions | 1.5 times more likely to develop folliculitis after recent skin injuries; hormonal changes can influence risk. |
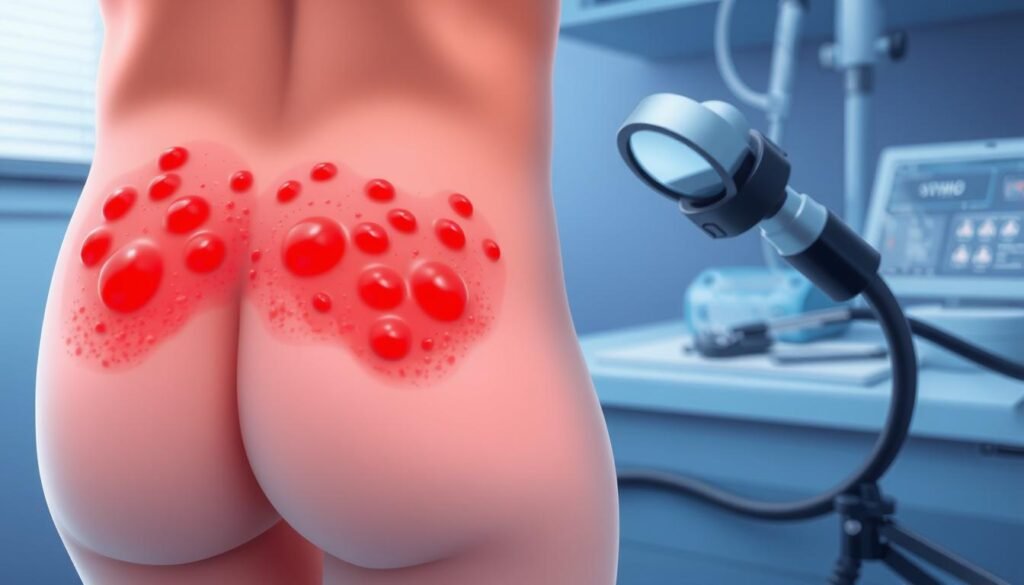
Symptoms of Butt Folliculitis
It’s important to know the symptoms of butt folliculitis for effective relief. This condition shows itself in ways that can upset those who have it.
Identifying Red and Inflamed Bumps
The main sign of butt folliculitis is small, red, and sore bumps on the skin. These bumps look like pimples and can really hurt. They often group together near hair follicles as a sign of inflammation.
Pus-Filled Follicles
Some red bumps can turn into pus-filled spots as the condition gets worse. These sores can burst open, leaking pus and causing swelling. In serious cases, bigger patches of skin might show inflammation signs. It’s vital to notice these early for treatment.
Itching and Discomfort
Intense itching and discomfort are common signs of butt folliculitis. This itching often comes with soreness in the affected spots. Early action against these signs is key to stopping them from getting worse and to lessen pain.

Diagnosing Butt Folliculitis
A thorough exam by a healthcare provider is the first step in diagnosing butt folliculitis. They look at the affected area closely. They check for symptoms and how bad the condition is. During the exam, they look for red, swollen bumps or pus-filled spots. These signs help them figure out if it’s folliculitis or something else.
Physical Examination by a Healthcare Provider
A healthcare provider will carefully check the skin on your buttocks. They look for visible symptoms. They might also ask about things that could trigger the condition. Such as:
- Recent hot tub or pool use
- Shaving habits or certain grooming products
- Past skin conditions
The goal is to tell butt folliculitis apart from other skin problems. A good exam can help find the right treatment.
Questions to Expect During the Consultation
Be ready for questions during your visit. They help diagnose butt folliculitis. You might be asked about:
- How often and how long you’ve had outbreaks
- Any creams or treatments you’ve used
- Your own and your family’s skin health history
The answers help the healthcare provider figure out the best treatment. They gather detailed info to understand your case better.
Treating Butt Folliculitis
To deal with butt folliculitis, use both home remedies and store-bought treatments. Acting fast can ease symptoms and stop them from getting worse.
At-Home Remedies and Self-Care Tips
At-home remedies are very helpful for mild cases. They include:
- Maintaining proper hygiene with gentle cleansing.
- Using antibacterial soap to reduce bacterial presence.
- Applying warm compresses on affected areas to soothe inflammation.
These easy steps can really help you treat butt folliculitis.
Over-the-Counter Treatments
If the problem stays, try some over-the-counter treatments. Look for products with benzoyl peroxide or topical antibiotics. These can fight the infection. Use them regularly for the best effect.
When to See a Doctor
Seeing a doctor becomes important when things don’t get better. Look out for these signs:
- Firm, painful bumps.
- Fever accompanying other symptoms.
- Symptoms that last longer than a few weeks, despite treatment.
Doctors might suggest prescription medicine. This can be more powerful against tough or deep-set cases of butt folliculitis.
| Treatment Type | Description | Use Case |
|---|---|---|
| At-Home Remedies | Proper hygiene, antibacterial soap, warm compresses | Mild cases, early-stage treatment |
| Over-the-Counter Treatments | Benzoyl peroxide, topical antibiotics | Persistent symptoms, self-treatment |
| Professional Consultation | Prescription medications, specialized care | Severe or worsening cases |
Preventing Butt Folliculitis
To stop butt folliculitis, it’s all about clean habits and smart clothes choices. By changing some daily routines, people can greatly lower their chances of getting this annoying issue.
Regular Hygiene Practices
Keeping clean is key in preventing butt folliculitis. Washing daily with antibacterial soap helps remove bad bacteria from your skin. It’s important to shower often, especially after a heavy workout or sitting for a long time. This helps keep sweat, oil, and dead skin away, which can cause folliculitis. When exfoliating, do it softly to keep the skin healthy and unclog pores, but don’t scrub too hard as it might irritate the skin.
Choosing the Right Clothing
Wearing the right clothes is vital for stopping skin problems. Choose clothes that are loose and made of fabrics like cotton or bamboo that let your skin breathe. Tight clothes that don’t let air through can rub your skin the wrong way and trap moisture. This can really raise your chances of getting folliculitis. For more tips on what clothes help skin health, here’s a good resource.
Effective Skin Care Routines
Good skin care habits can also help in preventing butt folliculitis. Use products that don’t clog pores, known as non-comedogenic. Trying natural solutions like tea tree oil can improve skin conditions if used regularly. For tips on home remedies, check this article.
| Preventive Strategy | Description |
|---|---|
| Regular Washing | Use antibacterial soap daily to keep the skin clear of bacteria. |
| Appropriate Clothing | Wear loose-fitting, breathable fabrics to reduce friction and moisture retention. |
| Gentle Exfoliation | Exfoliate gently to avoid clogging hair follicles while preventing irritation. |
| Non-comedogenic Products | Select skincare products that do not clog pores, promoting healthier skin. |
Comparison with Other Skin Conditions
Understanding the differences between skin conditions helps with proper diagnosis and treatment. A common mix-up happens between butt acne and butt folliculitis. These have different symptoms, affecting how they should be treated. Keratosis pilaris is also part of the conversation. It looks a lot like folliculitis but has a different cause.
Butt Acne vs. Butt Folliculitis
Butt acne, or acne vulgaris, is not common in that area. It usually shows up more on the face, back, and chest. It’s caused by clogged hair follicles and oil glands. Stress and hormones can make it worse. On the other hand, butt folliculitis affects the hair follicles directly. It usually gets better on its own in 1–2 weeks. It’s often due to friction, irritation, and bacteria.
The Role of Keratosis Pilaris
Keratosis pilaris causes small, rough bumps from too much keratin in hair follicles. It looks like butt folliculitis but isn’t caused by infection. It’s a common condition that affects the upper arms, thighs, and buttocks. Knowing these details helps compare these skin issues accurately for better skincare solutions.
| Condition | Type | Causes | Typical Treatment |
|---|---|---|---|
| Butt Acne | Acne Vulgaris | Blocked hair follicles and oil glands | Topical treatments, oral antibiotics, hormonal therapy |
| Butt Folliculitis | Inflammation of Hair Follicles | Bacterial infection, friction, irritation | Topical antibiotics, self-care |
| Keratosis Pilaris | Follicular Keratosis | Keratin buildup in follicles | Exfoliation, moisturizers |
Addressing these conditions means recognizing their unique signs and tailoring skincare to fit. A dermatologist can offer insights to make the right treatment plan. This improves skin health and raises awareness of one’s condition.
Impact on Quality of Life
Butt folliculitis can deeply affect a person’s quality of life. It can cause itching, pain, or irritation. These symptoms reduce daily comfort and disrupt regular activities.
Physical and Emotional Discomfort
Butt folliculitis also brings emotional issues. People may feel embarrassed or anxious about their symptoms. This may make them avoid social events.
Such emotional stress can worsen one’s quality of life. Finding the right treatment is crucial. It helps relieve both discomfort and distress.
Social Implications
The visibility of butt folliculitis leads to social challenges. Fear of judgment may stop people from enjoying activities like swimming. This can cause isolation and affect personal connections.
It’s important to seek support and effective treatment options. Solutions like those found here can boost confidence and social life.
Conclusion
Understanding butt folliculitis is key for those suffering from this skin issue. It causes discomfort with red or white bumps on the buttocks. These bumps are often due to irritated hair follicles. It’s important to know the signs of butt folliculitis and how it’s different from other skin issues.
Good hygiene, proper skincare, and wearing loose clothes help prevent it. Regularly getting rid of dead skin and using treatments like salicylic acid or benzoyl peroxide are also helpful. For a more in-depth approach, products from Exposed Skin Care might be worth looking into.
Those dealing with butt folliculitis should talk to a doctor for a personalized treatment plan. Understanding various treatment options is crucial. Taking steps to learn about and treat butt folliculitis can lead to better skin health.
